Post-Traumatic Stress Disorder
What is PTSD?
Post-traumatic stress disorder (PTSD) is a mental health condition that is triggered by a traumatic event. Traumatic events range across the spectrum and include actual or possible death, sexual assault, violence, abuse, combat, accidents, fires, terrorist attacks, natural disasters, and life-threatening medical diagnoses. The traumatic event may be experienced directly or witnessed; sometimes the simple knowledge of the traumatic event happening to your loved one or loved ones is enough to cause PTSD.
All traumatic events have effects on people. At times, trauma is felt more acutely and symptoms lesson over time with healing, yet at other times, symptoms intensify over time to the point of affecting day-to-day functioning in relationships, work and everyday life.
About 7 or 8 of every 100 people will experience PTSD at some point in their lives. While PTSD affects both men and women, women are more likely to develop PTSD.
What are the symptoms of PTSD?
Symptoms usually start within three months after an event, but they can take more time to develop and may even begin years after a traumatic event. Symptoms must persist for at least a month to qualify as PTSD.
Symptoms are often physical. Physical symptoms may include sweating, shaking, headaches, dizziness, stomach problems and chest pains. Because stress weakens our immune system, it may be that someone suffering from PTSD is more prone to various infections.
The DSM-5 — the handbook which healthcare professionals use to diagnose mental-health conditions — highlights four types of symptoms that must be present for someone to receive a PTSD diagnosis. These symptoms must actually lead to difficulty coping with important life components, such as work or relationships.
Intrusion symptoms: One or more must be present. These include nightmares, flashbacks and a sense of re-living the event, fearful thoughts, and severe distress when reminded of the event.
Avoidance symptoms: One or more must be present. These include refusing to discuss the traumatic event and avoiding situations and places that remind the person of the event.
Arousal & reactivity symptoms: Two or more of these must be present. These include general irritability and angry outbursts, difficulty sleeping, feeling tense and anxious, and being hyper alert to possible dangers.
Symptoms that affect thinking and mood: Two or more of these must be present. Symptoms include difficulty concentrating, inability to remember some aspects of the trauma, feeling detached from everyday life and like you are living in a fog, having a reduced interest in life and the things that used to interest you, feeling guilty, as well as other mental-health issues such as depression, anxiety, and the development of phobias.
Who is at risk for PTSD?
“Resiliency means that you are able to walk through trauma in a way where you emerge able to recover. ”
Not everyone who experiences trauma develops PTSD. In fact, people often experience PTSD symptoms initially after a traumatic event, yet for some, these symptoms subside over time. For others, the symptoms only intensify.
Various risk factors make a person more vulnerable to the development of PTSD. These include directly experiencing dangerous events and trauma; getting hurt; seeing other people hurt or killed; having experienced childhood trauma; experiencing extreme fear, horror and helplessness during the event; having a history of mental illness, substance abuse or both; having little or no social support after the traumatic event; and having significant stress occur after the traumatic event, such as loss of a job or home, loss of a loved one, or pain and injury.
Resiliency in the face of trauma does not mean that you are a robot who does not feel or experience the trauma. It means that you are able to walk through it in a way where you emerge able to recover.
While resilience is available to all people, some are able to access resilience more quickly due to various protective factors. The primary resilience factor is that of seeking support from family, friends and trusted professionals. Deciding not to walk through the trauma alone is most influential in moving someone towards resilience. This may take the form of reaching out to individuals or seeking out a support group.
Other protective factors that promote resiliency include learning to feel good instead of shame and guilt about your actions and response to the trauma. Another key resiliency factor is having life-giving coping strategies for walking through the pain and memories associated with the event. Lastly, remembering that it is normal to feel and experience fear when in danger or threatened aids in resilience. As the feelings of danger lessen, someone recovering from a traumatic experience is able to begin to feel safe in the world again, and to feel like they are equipped to respond effectively to any future danger that arises.
How is PTSD treated?
Treatment often consists of counseling and medication for the purpose of seeing that you regain your equilibrium and functioning as soon as possible. Counseling typically focuses on experiencing a supportive relationship where you can tell your story and begin to minimize the effects the trauma is having on you. This may involve developing coping strategies and re-framing the event — especially if you tend to view it with a lens of shame, believing that it was your fault. Medication may help to balance out biological changes and chemical balances that occur in our brains because of trauma.
PTSD & Veterans
PTSD is especially common in veterans; in fact, the rate of PTSD is found to be 15 times higher than in civilians, according to the National Alliance on Mental Health (NAMI). This makes sense when you reflect on the degree of trauma that is often experienced by veterans. While experiences range for each individual, sources of trauma that might impact veterans include military combat and assault, and the images, memories, hyperarousal, and effects that may stick with someone long after combat is over.
In this way, PTSD is often characterized and experienced by trouble sleeping, anger, nightmares, flashbacks, being jumpy, and alcohol and drug abuse. Naturally, when you are on such high alert all the time as military combat necessitates, it is hard to come down from this intense state of being to a more relaxed state. Your body and mind are still reeling from trauma and in a state of hyperarousal, and support is needed to heal and work through the experience. While it is normal for trauma to impact your life in a stressful way, you know that it may be PTSD when trauma continues to disrupt your life and functioning over time. The trauma of PTSD is unrelenting and continues to wreak havoc on your well-being.
PTSD for veterans may be felt by having intense reactions in the present to various triggers that are felt and experienced just like when you were physically in the traumatic situation. For example, hearing popcorn popping and finding yourself ducking for cover because your body responds like it is in danger. Or you may find yourself going about your business one minute and then re-living and visualizing the terror and trauma the next minute as if it’s happening in the here and now.
PTSD is often experienced alongside other significant challenges, including traumatic brain injury, substance abuse disorder, depression, and other health issues such as cardiovascular health. In this way, it is experienced mentally, yet trauma also affects the health of our bodies. Suicidal ideation and attempts are also a particular concern among veterans. Veterans who screened positive for PTSD were four times more likely to report suicidal ideation than those who did not, according to the American Psychological Association.
Thus, the effects of trauma are complicated and multifaceted, often lingering in their influence on someone’s life and affecting both mind and body. PTSD is not a mental health issue that typically just gets better on its own; rather, effective treatment and intervention is needed. Tragically, though, less than 50% of returning veterans receive any mental health treatment, according to Mental Health First Aid.
The good news is that there is help available for anyone experiencing PTSD and particularly for the veteran population. You do not have to continue to live in a state of terror as with quality mental and physical support, there is hope for healing and movement towards a more peaceful, fulfilling life.
Younger veterans may be more likely to seek help for PTSD than older veterans. Support is available for all veterans, and with effective treatment addressing both body and mind, there is great hope that anyone struggling cab move toward a place of healing.
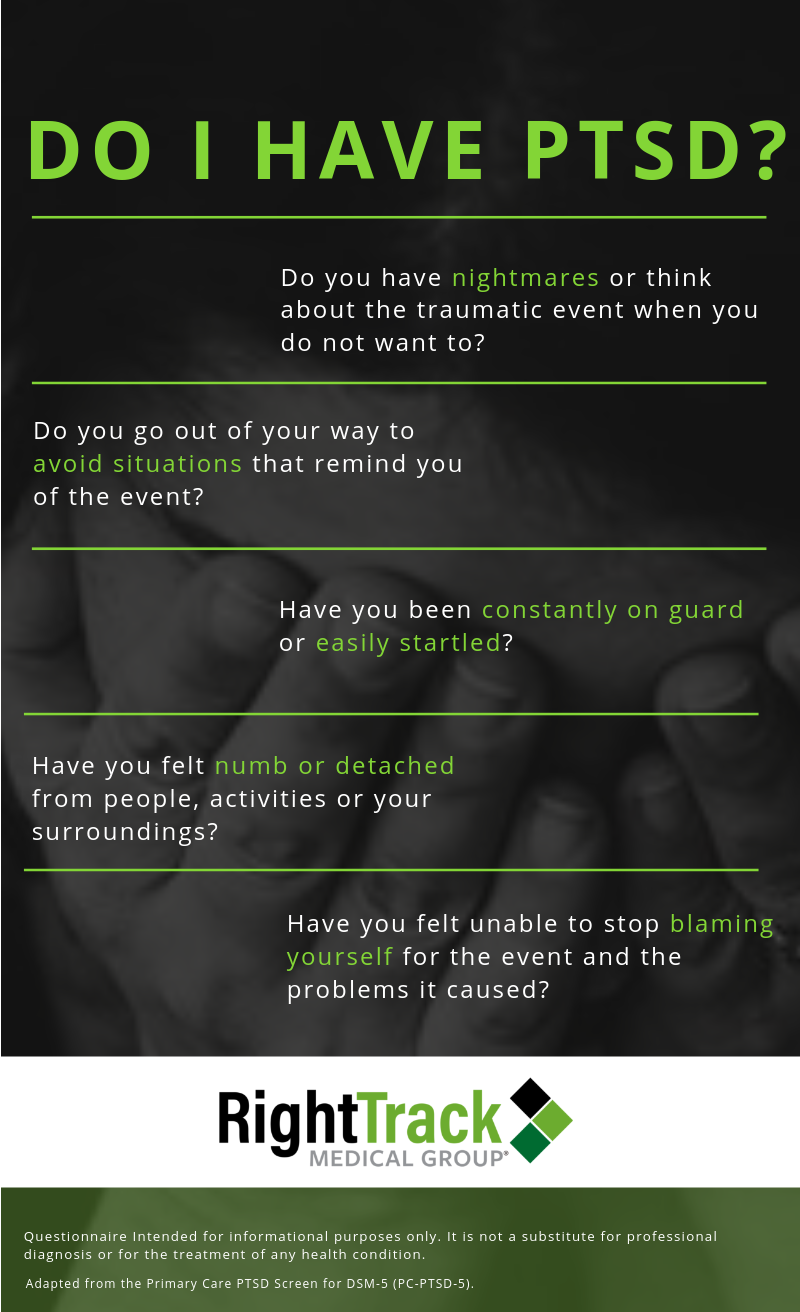
Do I have PTSD?
If you are finding yourself reeling from trauma, you are not alone. People typically know when a trauma they have experienced in the past is affecting them. An assessment by a mental-health professional can determine whether what you are experiencing is:
An acute stress reaction
Difficulty adjusting to a traumatic event that has occurred
A true PTSD diagnosis
It is normal for trauma to affect people, but its effects can be mitigated through appropriate mental healthcare and support.
If you or someone you care about is experiencing the pain and after-effects of trauma, seek help and support quickly. By doing so, you may help prevent full-blown PTSD from developing.
If you are already in the throes of PTSD, experiencing its intensity and the havoc it is causing your life, reach out for help right away.
Schedule an evaluation today at the Right Track Medical Group clinic nearest you.
PTSD Resources
The Mental Health Needs of Veterans, Service Members and Their Families: American Psychological Association (APA): https://www.apa.org/advocacy/military-veterans/mental-health-needs.pdf
This resource from the APA looks at the invisible wounds of war.
Post Traumatic Stress Disorder: Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967
This guide by the Mayo Clinic, provides an overview of PTSD, symptoms and causes and diagnosis and treatment.
Post-Traumatic Stress Disorder: National Institute of Mental Health: https://www.nimh.nih.gov/health/publications/post-traumatic-stress-disorder-ptsd/index.shtml
Provided by the National Institute of Mental Health, this guide includes information on PTSD, different symptoms of PTSD and also additional information such as how children react different, why someone may experience PTSD and others do not and also information on how to help someone who has PTSD.
PTSD Screening Instruments: U.S. Department of Veteran Affairs: https://www.ptsd.va.gov/professional/assessment/screens/index.asp
The U.S. Department of Veteran Affairs also home to the National Center for PTSD, provides several brief questionnaires that may identify people who are more likely to have PTSD.
PTSD: What you need to know: Medical News Today: https://www.medicalnewstoday.com/articles/156285.php
This guide by Medical News Today on PTSD explains symptoms and diagnosis, causes, risk factors, treatment, self-help tips, complications and prevention.
PTSD and Veterans: Breaking Down the Statistics: Hill & Ponton Disability Attorneys: https://www.hillandponton.com/veterans-statistics/ptsd/
This source looks at some key statistics around veterans and mental health.
Troubling Veteran Mental Health Facts and Statistics that Need to be Addressed: National Veterans Foundation: https://nvf.org/veteran-mental-health-facts-statistics/
This article looks at the barriers many veterans face will seeking mental health treatment.
Veteran’s & Active Duty: National Alliance of Mental Health https://www.nami.org/Your-Journey/Veterans-Active-Duty
This guide looks at the mental health struggles of veterans.
Veterans & Military: Mental Health First Aid: https://www.mentalhealthfirstaid.org/veterans-military/
In this resource, Jeannie Campbell, National Council Chief Operating Officer and Navy Veteran, describes the importance of addressing veteran’s mental health and how Mental Health First Aid can help.
By Elizabeth Burton, LPC, EdS, NCC for Right Track Medical Group
This article is provided for information only and is not a substitute for diagnosis or treatment by a mental-health professional.